Licence to Pill
Graham Panther on madness, choice and how lived experience becomes policy
There’s a joke from Samuel Goldwyn that goes: anyone who sees a psychiatrist should have their head examined. It sums up the transactional nature of power – how in some ways psychiatrists are like any other guru – that is, they have power because you give it to them. If you’re feeling helpless, here’s someone you can imagine has all the answers you seek.
Unlike your average guru though, psychiatrists – and mental health services in general – also have another kind of power, one you can’t easily revoke when you decide you want to find help some place else. As part of the medical establishment, they have a great deal of institutional authority, including the power to suspend your human rights, and to force you to receive treatments against your will.
If you disagree with your psychiatrist, that’s just another sign you’re crazy, right? But what if that’s not true? What if over time, our insistence that ‘doctor knows best’ has become a barrier to understanding madness? These aren’t easy questions to answer, but they have far-reaching implications for how we view mad and distressing experiences in general, whether you’re at the pointy end of the system, or picking up your first script of antidepressants.
Some say we’re on the cusp of a collective, global mental health crisis. The prestigious Lancet journal called the worldwide rate of mental health issues “a striking and growing challenge” to health systems (Whiteford, et al, 2013). New Zealand’s Mental Health Commission says we need to increase access to mental health services over the next decade, even as funding will become “tighter and more difficult” (Mental Health Commission, 2012). Perhaps some breakthrough in medical science will solve this looming mental health dilemma? That’s certainly the promise of each new antidepressant or antipsychotic on the market: more benefits, less side effects.
At the same time, however, there’s something of a crisis within psychiatry itself, and some are starting to question the basis of its authority. Indeed, amidst the dire projections, the Mental Health Commission says our best hope is a society-wide approach to mental wellbeing. Following their lead, perhaps it’s not a medical breakthrough we need, but a social one.
Let’s look at the main tool in the psychiatric toolkit: medications. Recent studies show that drugs are no more effective than placebo for treating depression, and this applies both to the mild and severe ends of the spectrum (Andrews, 2001; NICE, 2009; Fournier et al, 2010). Take that in for a moment. Stick to the sugar pill, and you’ll likely get the same outcome.
As for the things we call ‘severe mental illness’ – hearing voices, delusional thinking – a whole series of trials has found the effects of drug treatments to be “disappointingly limited” (see Bracken et al, 2014). Then consider the catastrophic health effects of long-term antipsychotics, including heart disease, liver failure, and a host of other issues. What happened to ‘first do no harm’? In the case of ECT – shock treatment – one study found that “sham ECT” was actually more beneficial than the real thing (Rasmussen, 2009). Without the risk of memory loss to boot.
Now, this isn’t to say these treatments don’t work, per se. People on the real pills and people on the placebo both got better – just not because of what’s in the pill. Pat Bracken, one of the founders of the Critical Psychiatry Network, has an interesting take on this. I cornered him at a conference last year, after his keynote completely shook my smug, preconceived notions about his profession. We talked about this placebo thing - how maybe it’s the sense of hope you get from receiving treatment, or maybe the benefit of a good relationship with your treating team. And how maybe people get better because, well, people get better.
I’ve worked in the mental health sector for almost a decade – setting up and evaluating services, trying to figure out what really works – and I’ve met a whole lot of people navigating their way through the system. In my experience, humans are actually a highly resilient bunch – and, contrary to popular thinking, picking up a diagnosis is just as likely to make you stronger, not more fragile, as you test your own limits and realise what you can come back from.
In our society, we place a great deal of value on certainty. When we think something is irrelevant we say, ‘well that’s neither here nor there,’ because if something can’t be pinned down or classified, we see it as useless. The expert in any given subject is the one who can make the most definitive statements about it. In many fields, this approach is extremely useful. General health, for instance, where of course you want a doctor who can say with certainty what each part of your body does, and how various ailments will afflict them.
Mental health is different, though. Can you really make definitive, objective statements about something as subjective as your state of mind? We’ve spent the last 300 odd years trying to do just that. The results have been mixed, at best. Studies show that even senior psychiatrists can only agree on a person’s diagnosis about 50% of the time (Kirk & Kutchins, 1994; Van Os, 1999). Keep in mind that your diagnosis has major repercussions on what treatments you’re given, and what supports you can access from multiple government departments – health, social welfare, corrections, education, and more. So if the psychiatrists can’t even agree, why continue to invest so much authority in their findings? Because in our culture, the alternative is scarier. We’d rather have experts who are wrong half the time than no experts at all.
Imagine a different model of expertise, one that has more room for subjectivity. Ever desperately needed a drink at the end of a long workday? Or passed a lost weekend on illegal substances to feel better about life for a while? At least one prominent psychiatrist, University College London’s Joanna Moncrieff, says that’s how we should think about prescription psych drugs too. We’ve all heard about the chemical imbalance that supposedly causes depression, or psychosis. But ask any psychiatrist, and they’ll tell you: this is still just a theory.
Moncrieff argues that we’re approaching psych drugs all wrong. Instead of saying “You have a brain imbalance, and this pill will fix it”, we should say: “We don’t really know what’s going on for you, but this pill will make you feel different. You might prefer that to how you currently feel, or you might not.” Once again, the big idea? You get to choose.
Increasingly though, we’re actually taking away people’s choices. Recent studies show that in New Zealand, rates of compulsory treatment are unusually high by international standards, and they’re steadily rising (O’Brien, 2014; Ministry of Health, 2012). All this throws up a question: is ‘compulsory treatment’ an oxymoron? If the most important part of the treatment is that you see value in it, why foist it on to people who don’t want it?
The elephant in the lock-up is, of course, the question of safety. Compulsory treatment is supposed to be used only when someone is considered a risk of harm to self or others. Fair enough, but this is extremely difficult to judge, and my opinion is that we err on the side of risk aversion at the expense of human rights. If you’ve received a diagnosis, you’re less likely to be violent than the general population. You’re massively more likely to be a victim of violence than a perpetrator.
Yet in my work, I’ve seen some pretty flimsy justification for compulsory treatment, including not showering daily. In other cases, it seems like the main criteria is simply being unusual, even if it’s harmless. I met one man who’d been picked up by the authorities because he converses with his wife who’s been dead for years. He feels her hand on his arm when he’s anxious, and takes great heart in her presence, but he’s been forced to receive monthly injections to try to stamp out these deeply private moments, against his better judgement.
Why aren’t studies like the placebo trials causing shockwaves in mental health practice? The issue, again, is power. Or rather, the blind spots that can manifest when power meets expertise. A 2007 study by Mitchell and Selmes showed that, after 4 weeks, most people actually stopped taking their prescribed drugs. They didn’t tell their doctor this; and despite stopping the pills, most of them got better anyway. But from the doctors’ point of view, they see their patients – who to their knowledge are still taking the drugs – get better. So they think: the pills work for most people. This well-meaning conviction can be a barrier to understanding their clients. To quote Alan Watts: ‘here let me help you’, said the monkey, putting the fish safely up a tree.
Bracken says it’s the ‘soft and fuzzy’ stuff that’s more important than any pill or psychological technique in promoting recovery: hope, connection with others, and a chance to find meaning in your mad or distressing experiences. The last point includes the ability to define your experience in your own words.
For some, the medical terms and diagnoses may resonate. For others, it could be all sorts of things – and that includes the possibility that your ‘symptoms’ might actually be something you see value in, like the man hearing from his dead partner. Or a colleague of mine who’s grown up knowing that the voices he hears are a direct connection to his whakapapa. Or another colleague who has multiple companions, traveling with her always – one who’s a pain in the arse, and one she finds particularly insightful in tough times.
*
In my case, I came to view my own ‘out there’ experiences as a philosophical challenge, one that took everything I had to meet. In my early twenties, like everyone else, I went through a messy breakup. Around the same time, I had a life-threatening experience, and the combined stress led to a prolonged period of what I can best describe as: being a little out of it. Completely sober, I’d get these trippy experiences where time and space would collapse in on each other. The rest of the time I’d just feel monumentally panicked, which is about as fun as it sounds.
Naturally, I went to see a psychiatrist. Before that I’d tried two separate neurologists, and neither had found any anomalies on the various scans they’d done. This didn’t deter the psychiatrist from his conviction that my trippy experiences must have been biological in cause. He told me straight up I probably had “lasting brain damage”, cause unknown.
This made me feel exactly as hopeless as you might think, for a very long time. After a few months, once I’d picked myself back up from that devastatingly casual life sentence, I chose to stop seeing him. I was lucky enough to have that choice, where others might not.
I went down a different path, one that eventually involved jumping out of a plane (with a parachute), followed by months of a gorgeous, background euphoria, and an ongoing epiphany about how I wanted to approach this whole ‘being alive’ thing. Since then, I’ve never found any personal value in the idea of ‘mental illness’. Even if the “brain damage” thing hadn’t been totally bogus – even if there had been a magic pill instead of months on end of increasingly bewildering side effects from the ones that were prescribed to me – with hindsight I’d still choose my story of transformation, any day.
I’m not entirely sure why, but I went back to the same psychiatrist one last time, armed with this self-reflection and renewed confidence, maybe just to see what he’d make of me. His response to my triumph was: “yes, of course, I could have told you that would work”. For want of a better term, he went on to ‘psychsplain’ what I’d done, with some mechanical metaphor about switches getting stuck. None of this apparently self-evident knowledge did he feel was worth sharing two years earlier, when I’d have taken any scrap of hope.
But then, why would he? The moment I stepped into his office, my experiences became symptoms, and my state of mind became a disease. That’s all he had to work with. The best advice I got in that time was actually from my dad, who had little frame of reference from his own life (as far as I know) but offered, “hey, some people pay a lot of money for experiences like that. Can you try to enjoy the ride?” I didn’t have an answer for him then, but it turns out – yeah, eventually I could.
Whenever I share this part of my life, I’m careful to say: it’s just one story. Your mileage may vary. For some people, medical treatment may be part of the answer, including great doctors who are a credit to their profession. For others, a different path awaits. The key, as always, is choice – and offering meaningful choices is still something mental health services need to work on. We won’t get there until we stop pretending there’s only one ‘real’ way to understand madness and distress.
The evidence says hope and meaning are key, but it doesn’t say they’re easy to find. They might be the hardest-won things you’ll ever earn, just as they are for the rest of the population. This is especially true for those whose voice in society is already devalued by sexist, or racist, or homophobic, or transphobic, or classist social structures. Many commentators have pointed out how the notion of ‘mental illness’ leaves no room for social context, locating the problem in the brain of the individual, when the main issue may in fact be intimate partner violence, or societal prejudice, or systemic disadvantage.
There’s a particularly striking case in point that exists in living memory. Until 1986, same-sex attraction was classed as a symptom of ‘mental illness’ (DSM-IV, introduced at that time, finally did away with ‘ego-dystonic homosexuality’). As Bracken notes, this didn’t change because of some brain science discovery. The change was a social one, led by LGBTQIA people. Doctors are no longer the experts on being gay. Gay people are.
Imagine a world in which the experts on madness are people who’ve experienced it. Fact is, there is in fact a lesser-known social movement that has sought to achieve just that: the Consumer Movement. Alongside the great movements of the past 60 years, people who had used mental health services (‘Consumers’) banded together to advocate for a new way of doing things. Despite the rise of compulsory treatment, their work over the past few decades has driven major gains for the human rights of people accessing mental health services. We didn't even have a word for recovery in mental health until the movement said: we’re living proof that you can get better.
Now recovery is written into high-level policy. The Consumer Movement showed people that you can have a great life, whether your mad experiences are something ongoing you weave into your sense of self, or something transitory you leave behind.
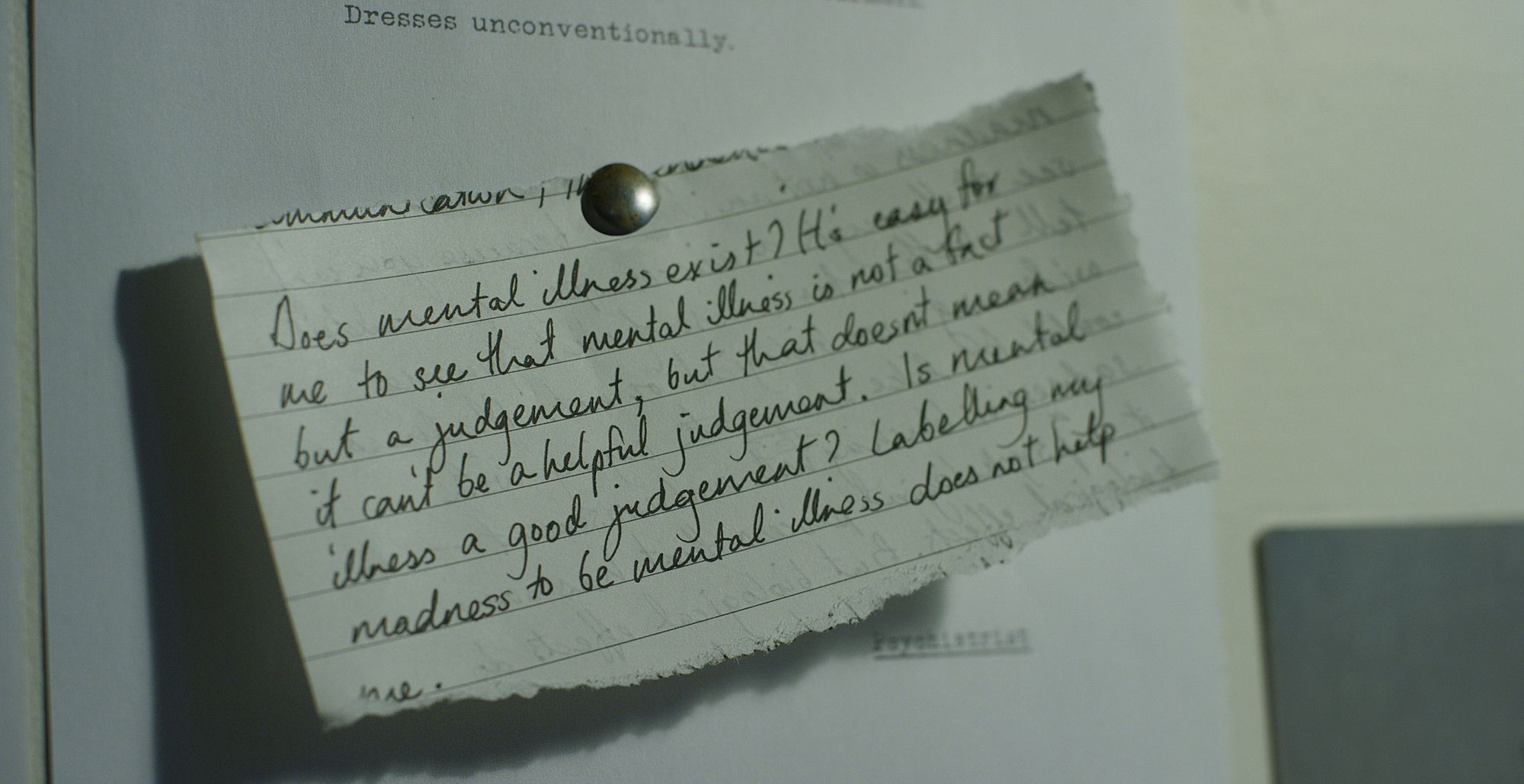
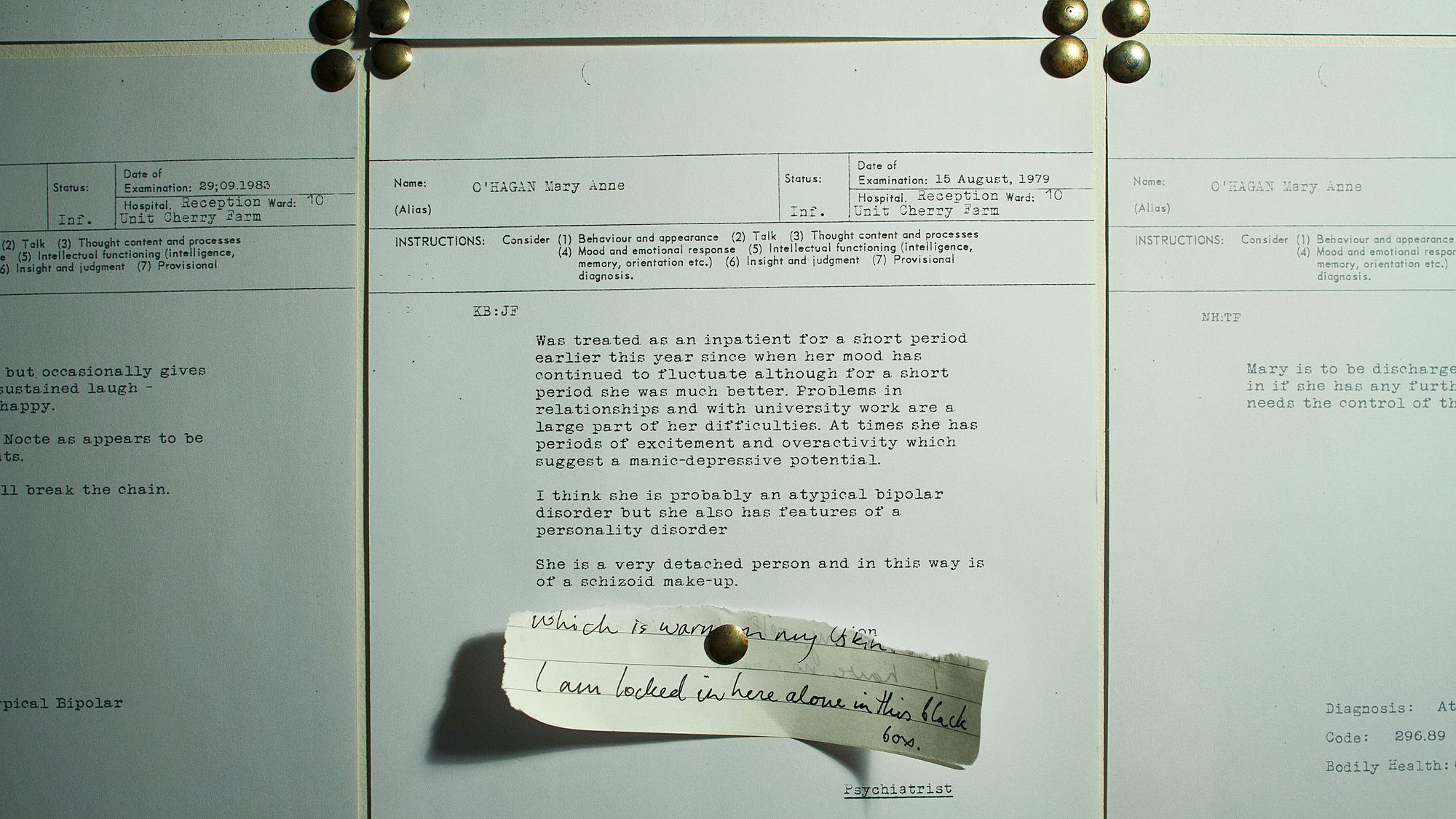
If we’re to build on these successes, it'll continue to be led by people with mad experiences. It’ll involve artists like Lena Dunham exploring obsessive-compulsive behaviours as just one part of a rich, multi-layered TV character. It’ll involve authority figures like Australian Federal Court Justice Shane Marshall, who recently came out about experiencing depression while on the bench. Or leaders like New Zealand’s own Mary O’Hagan, who spent years in and out of psych wards through her twenties, and has played a major role in the Consumer Movement here and abroad.
Madness Made Me from Loading Docs on Vimeo.
O’Hagan is the subject of Madness Made Me, a new short doco by director Nikki Castle, part of the New Zealand Film Commission’s Loading Docs scheme. As the film explores, O’Hagan’s life and work point the way toward a new way of viewing madness: as a thing of value, and a source of knowledge. As our first openly mad Mental Health Commissioner, she has helped shape a more responsive mental health sector, and she continues to advocate for the rights of people using mental health services. Bracken cites O’Hagan as a point of inspiration – and many other clinicians are willing to think critically about the primacy of the medical framework in which they operate, which bodes well for the future.
Medical expertise is supposed to help us better understand madness. But if it’s considered the only legitimate way of making sense of madness, it becomes a barrier to understanding. New Zealand studies show that nearly one in two of us will qualify for a diagnosis at some stage in our life, which means we’ve got a lot more in common then we think (Oakley, Browne, Wells & Scott, 2006). We now need to find new ways of talking about mad experiences that recognise our common ground, without minimising the experiences of those who’ve had it particularly tough. In my view, this starts with recognizing one simple fact: that madness is a human experience, with all the terror, and the joy, that human life can bring.
References
Andrews, G. Placebo response in depression: bane of research, boon to therapy. Br J Psychiatry 2001; 178: 192–4.
Bracken, P., Thomas, P., Timimi, S., Asen, E., Behr, G., Beuster, C., Bhunnoo, S., Browne, I., Chhina, N., Double, D., Downer, S., Evans, C., Fernando, S., Garland, M., Hopkins, W., Huws, R., Johnson, B., Martindale, B., Middleton, H., Moldavsky, D., Moncrieff, J., Mullins, S., Nelki, J., Pizzo, M., Rodger, J., Smyth, M., Summerfield, D., Wallace, J., and Yeomans, D. 2012. Psychiatry beyond the current paradigm. BJP 2012, 201:430-434.
Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 2010; 303: 47–53.
Kirk, S. & Kutchins, H. (1994). The myth of the reliability of the DSM. Journal of Mind and Behaviour, 15, 71–86. (www.academyanalyticarts.org/kirk&kutchins.htm)
Mental Health Commission. 2012. Blueprint II: How things need to be. Wellington, Mental Health Commission.
Mitchell, A., and Selmes, T. 2007. Why don’t patients take their medicine? Reasons and solutions in psychiatry. Advances in Psychiatric Treatment (2007), vol. 13, 336–346
National Institute for Health and Clinical Excellence (NICE) (2009). Depression: The Treatment and Management of Depression in Adults. NICE Clinical Guideline CG90. London: NICE (http://guidance.nice.org.uk/CG90).
Oakley Browne, M.A., Wells, J.E. & Scott, K.M. (Eds.). (2006). Te rau hinengaro: The New Zealand mental health survey. Wellington: Ministry of Health.
Van Os, J., Gilvarry, C., Bale, R., Van Horn, E., Tattan, T., White, I. et al. (1999). A comparison of the utility of dimensional and categorical representations of psychosis. Psychological Medicine, 29(3), 595–606. www.ncbi.nlm.nih.gov/pubmed/10405080
Whiteford HA1, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJ, Vos T. Lancet. 2013. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Nov 9;382(9904):1575-86.