A Second Chance: Of Hearts and Hospitals
Max Harris was 26 and enjoying a dream job working for Helen Clark in New York when he fainted in his apartment. It was the start of a chain of events that changed the course of his life: leading him away from the UN and into emergency wards, MRA machines and ultimately, a surgical theatre.
It’s almost pitch black, at about 10.30pm on a Thursday night, in the middle of nowhere somewhere between New York and Baltimore. I walk out across the petrol station while the bus takes a rest break, and the cicadas aren’t just humming – they’re screeching. I look around. It’s desolate and dark.
I’m meant to be in New York, coming to the end of an internship with the office of Helen Clark, Administrator of the United Nations Development Programme – a dream job. Instead I’m on a Megabus heading to Baltimore, on my way to Johns Hopkins Hospital, about to see the doctor responsible for discovering a rare condition called Loeys-Dietz Syndrome and an expert in heart surgery.
How did I get here? And how did it come to this?*
From December 2013 to January 2014, I attended the wedding of my friend, Akif, in Pakistan. It was a unique experience, made more memorable by the fact that for 10 days, 15 friends of Akif’s were largely confined to an apartment in Karachi because of the security situation in the city. The apartment was in the Defence quarter, opposite an ostentatious shopping mall. A McDonald’s had its grand opening while we stayed there – but the apartment was otherwise surrounded by an expanse of desert-like terrain, with the shadowy shapes of Karachi’s skyline only barely visible in the distance.
We all went a little crazy biding our time until wedding events. There were rich conversations: on New Zealand politics and law, on the books we had, on the future. But even with the best company, most people get fidgety after that much time in an enclosed space. We were no different. We were driven to activities that would’ve bordered on the looking wacky to anyone watching from the outside: building towers of bottles on glass tables, and narrating shadow puppet shows before we went to sleep at night – three per bed, with a hessian sack in place of bedding for one of us.
On one of these days, with the fan whirring in the background, the only doctor in our group, Andrew, turned towards me across the room. He looked at me – as I stretched – and, joking in part, mentioned that in some ways I looked like a person with an unusual disorder called Marfan Syndrome. He asked me whether I could do certain things – like whether my thumb poked out if I clenched it under my fingers in a fist-like move – and made some comments about my limbs and my chest. “You should get it checked out next time you go to the doctor,” he said – or words to that effect.
Marfan Syndrome is a genetic connective tissue disorder. It tends to arise in people who are tall, who have long limbs, spidery fingers, and slightly odd-shaped chests – though the symptoms and diagnostic testing require much more than this. If undetected, it can lead to sudden heart problems.
At the time I laughed it off. My friend was only half-serious. And my quick Googling revealed body shapes that, while resembling mine, looked much more unusual.
In hindsight, I’m extremely grateful to Andrew for his off-hand remark. In some ways, it was in that apartment in the Defence quarter of Karachi, that all of this began.*
Last year, as part of my Master’s degree at the University of Oxford, all students were asked to organise an internship, a “summer project”, to round off our studies of public policy. After some brainstorming, I decided that my ideal position would be with Helen Clark, the head of the UN’s Development Programme and former Prime Minister of New Zealand – a progressive leader I’ve long looked up to. With the support of the Blavatnik School of Government, I managed to arrange an internship in New York for two months from late June until late August 2014.
Fast forward to early August – and I’m having the time of my life. I’m working with intelligent, friendly people, passionate about making a difference in the world in a rigorous way, and at scale. Topics at work span public health (in particular, HIV/AIDS), climate change, poverty reduction, and how organisations can best anticipate the future (“strategic foresight”). On the weekends I’m roaming coffee shops and independent bookstores – Double Dutch Espresso, McNally Jackson’s, 9th Street Espresso, the Housingworks Bookstore – and finally coming to love a city I’ve always wanted to like but never fully wrapped my head around.
On one Monday, though, as I’m walking out of a subway in East Village on my way to the bookstore Bluestockings when I feel a fleeting but sharp pain in my chest. I’ve become quite an anxious person in recent years, so my mind leaps to the worst case scenario. I slow down, take a break, and decide to buy some water. I walk on for a while, but the pain returns, briefly. I text my Mum, back in New Zealand – a nurse, and a wonderful person who knows my anxiety as well as she knows about addressing pain. She calls, asking me whether I've been eating and drinking and sleeping well, and tells me to stay in touch. Inside Bluestockings, I can’t really concentrate. I feel weak and a bit faint in the New York heat. I remember sitting on a bench outside the bookstore for at least a few minutes, and then gradually getting to my feet to take small steps towards the subway home.
At home, my kind flatmate Mike, a medical student doing a period of practical training in New York, agrees to talk about how I’ve been feeling. He listens to my heart and mentions that everything seems and sounds relatively normal – noting, I think, that the issue could be to do with my aorta, but commenting that at 26, any problems would be unusual. “Keep tabs on it, though,” he says. In the preceding few months, Marfan Syndrome had come to my mind several times (during occasional chest pains in Oxford), and it returned to my thoughts again. Had Mike heard of it, I ask, and what did he think? He laughs, surprised that such an unusual disorder would come to mind. He expresses scepticism, but also looks equivocal. He can’t be sure, but it’s certainly unusual.
I found myself getting blurred vision as I sat on the side of my bed. This was the worst I could have feared, I thought.
On Sunday – unfortunately the day after Mike moved out of the apartment – I blacked out. The night before I’d read a tragic story in the New Zealand Herald about a young New Zealander who died suddenly in Sydney of a rare connective tissue disorder. He looked tall and slim, and I couldn’t help think of Marfan Syndrome. I woke up worrying, and after a bit of an Internet review, which I tried to filter for more reputable sources, I found myself even more concerned. What if I had the syndrome, and I was about to be suddenly struck down by it? I read somewhere that severe episodes must be caught within a couple of weeks if they are to be managed (and sometimes they can have more immediate, catastrophic effects), and I felt like my pains had been occurring for the last week or so. Whether because of anxiety or something else, I found myself getting blurred vision as I sat on the side of my bed. This was the worst I could have feared, I thought; but at the same time I tried to stay calm.
Some water might bring some relief, I thought. It was what my Mum had always recommended. I got up and took a few paces down the hallway towards the kitchen. At some point I realised I wasn’t going to get there. I turned back towards my bedroom, and next came a few moments that I won’t ever be able to piece together. Presumably after my legs buckled from under me, or perhaps after I fell backwards. In any case, I was fortunate to hit my head on the floor at a force not strong enough to cause any damage, but distinct enough to bring me back to consciousness. I stared back into my bedroom, startled and a bit bemused, and it took me a few seconds to realise that I had fainted or somehow lost consciousness. “I think I just fainted,” I said to my room-mate, Matt, who grabbed me some water before he had to race out the door. Mothers and others must think alike: water is the remedy for most ailments.
I still thought that going to the hospital would be an overreaction – a lot of people faint, for a lot of reasons, right? – and in the back of my mind was a worry about the cost of hospitalisation in the US. But when I sat down and felt a numbness in parts of my body (my foot and my arm), and began losing vision again in my left eye, I thought that the situation was probably serious enough to start making inquiries about medical options.
What followed – between that moment and getting to the hospital – was pretty farcical, and wouldn’t happen in a country with public healthcare. I wanted to check the emergency health insurance kindly provided by the Blavatnik School of Government would cover my hospital visit. It took 20 minutes on Skype to get in touch with a friendly-sounding man, who told me the insurance would cover my hospitalisation, and that they would now find a hospital with which they had cover and call me back. I waited, I think, for another 40 minutes, all the while sitting at my bed and playing out different scenarios in my head. I decided to play some music by Liam Finn to calm me down – I had seen him play an outrageously good live show in New York only a fortnight previously. His song, Second Chance, was ringing in my head:
You stand around your haunted home
Those demons won’t leave you alone
Don’t forget me when you grow old
Remember! Remember! Remember!
I looked at my clock. Almost an hour had passed. I decided to call the insurers again, and a lovely man named Kevin told me that I should go to Mt Sinai Hospital, and that I shouldn’t worry about being covered.
In another moment that was as comical as it was farcical, I realised that the mobile data on my phone plan in the US had not been working, though I had paid for it. I suddenly thought that I should see if this could be fixed – if I was about to go into hospital, I’d need a way to speak to people, and perhaps I could get hold of them on Skype.
“Hi, uh, I have a bit of a medical situation,” I stammered – my Kiwi tendency towards understatement probably coming through – as I leapt into a taxi I’d hailed.
An upbeat, male call-centre voice replied: “What is the problem with your phone, sir?”
“Ah, yeah, I don’t have Internet though I’ve paid for it. But I really need Internet: I’m about to go into hospital and need it to get hold of people.”
In words that I am not making up, and which show the ills of a society that prioritises rule-based bureaucratic interaction over human dialogue, the man responded: “So, let me summarise: you have a problem with Internet on your phone …”
If I hadn’t been so worried, I would have laughed. As it was, I let out a small smile. Unfortunately, my Internet couldn’t be fixed during the course of that taxi ride. But I was too focused on the hospital to really care. Moments later, I checked myself into the emergency ward of Mt Sinai Hospital, New York.*
I had been expecting to wait for some time, but I was impressed with the speed at which I was moved into a bed in the Emergency Department. I was given some preliminary interviews, told I would be getting various scans done, and fitted out with a gown. (I later discovered that I had put the gown on the wrong way round, with openings – usually exposing the back – that revealed my chest. I got some funny looks, but as anyone who has spent time with me knows, there was hardly much of a muscular spectacle to behold there.)
The first day in hospital flew by. I had curtains around my bed and I lay back, relaxed, looking out into the main central medical desk in the department – a positioning that gave me the curious feeling of being an audience member peeping at actors preparing to go onstage. It was especially curious being able to hear, occasionally, the doctors discussing my case, on the phone or with each other: “Uh, yeah. We have a 26 year-old male, who’s had a syncopal episode, with marfanoid habitus …”
That day was full of slightly absurd episodes. There was the rap-battling, freestyling male-and-female nurse duo, who were constantly sniping at each other – with my highlight being the male nurse’s line, “If I was a donut/You’d wanna glaze me”. There was the drunk man – whose severe alcoholism, to be sure, was no laughing matter – who croaked out for a urine bottle, only to use it, put it down next to his bed with no lid on it, and then swat it over, spilling the contents all across the floor in front of me, where it stayed for a good 10–15 minutes, painting the floor yellow. There was the CT-scan room, a room that I thought would be full of sterility and technology – but that was brought alive by the sound of loud hip-hop music when I was taken in on a stretcher. (“They always have the best music in here,” deadpanned the staff member tasked with pushing my stretcher.) I also couldn’t shy away from hearing the rectum examination that had to be done on the man with whom I was sharing my right curtain. I’m sure this procedure was much worse for him, since it had to be done essentially in public, with only curtains shielding him from the other patients. Welcome to the hospital.
Those stories may imply that I made light of the experience. I didn’t. When I made contact with the outside world – calling my friends Alaister and Mitch, or my parents – I found myself choking up. It was only in talking to people not in the hospital, and hearing their reactions to what happened and what was happening, that I started to realise the seriousness of the situation.
Important news came towards the end of the day, around the time my friend Mitch visited: one of the scans revealed that I had an enlarged aorta, or aortic aneurysm. And the doctors were all seriously considering the possibility that I had Marfan Syndrome, with all of them being impressed that I had a friend that pointed out the possibility to me. The fact that the enlarged aorta was being investigated alongside Marfan Syndrome was significant: if I had Marfan’s, the enlarged aorta would be considerably be more problematic, as the connective tissue disorder at the heart of Marfan’s would make it more likely that the aorta might tear (through a “dissection”), with potentially deadly consequences. The doctors began to talk about surgery, one even using the term “life-threatening” to describe my position - a term that stayed with me. They said that I would definitely have to stay overnight.*
I was moved the next day to an observation room with three other patients. There was still a chance that I would have to go into surgery. A friend (my girlfriend’s brother), Paul, took time off work to chat and bring me a phone charger and some headphones. I also struck up conversation with a lovely older woman, Gladys Brodsky, who was dealing with the after-effects of heart surgery. On my second day, she invited me over to her side of the room to share a hospital lunch.
Gladys was a Jewish artist who had spent her life in Woodstock. She was grey and frail, but had a certain elegance that remained even as she faced up to the vulnerability of being in a hospital. In her own way, she was charming. She spoke about Bob Dylan, Joan Baez, and others living in Woodstock; Israel and Palestine; and her past days as a women’s rights activist. “If all men were injected with oestrogen at age 13, and took on a few female characteristics,” she mused at one point, “I think the world would be a lot different.”
She spoke lovingly about her father (“a socialist, not a communist”), who used to hold learning evenings every Tuesday with members of the community on political topics (“only the men”, she noted, when I asked if women went too). “He was a genius,” she said wistfully. I told her that I sometimes felt similarly about my own father, and this sparked a further discussion about whether our conception of “genius” is gendered. We both concluded it probably was, and that our mothers were probably geniuses, too. We touched on bigotry, as well – and Gladys spoke eloquently about how racism lies “deep in the bones” of the United States.
For the first time in my life, I thought about the beauty of good conversation, and how much I enjoyed it. In the listening and learning that exist in a conversational dialogue, in the symmetry two or more people can find when each shares a part of themselves, in the spontaneity that can gush out when two people are truly comfortable – there is something special.
In between this conversation and the visits of other friends, there was sobering medical news. There was further talk about surgery, which my mother (calling from New Zealand) cautioned against going into suddenly. The doctors wanted to continue with testing. They told me that MRA imaging was going to be done next, to try to resolve discrepancies in the measurements of my enlarged aorta.
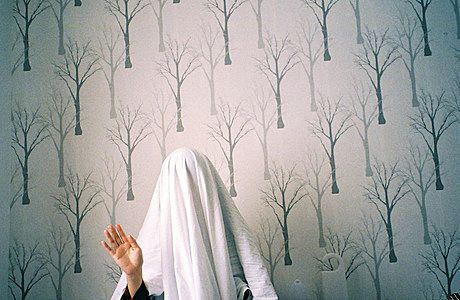
Max at Mt Sinai Hospital in New York.
Perhaps in an effort to steel myself against these sombre updates, or to find some semblance of support as I tried to maintain mental strength, I began to build some rapport or warmth with the staff at Mt Sinai. Dr Weiss always left me feeling buoyant, clasping my hand after delivering updates. A friendly young transporter inquired about why I was in hospital, and when I mentioned that the doctors were interested in Marfan Syndrome, he made me feel better by referring to a young basketballer, Isaiah Austin, who was set to be drafted into the NBA, only to have his career cut short by the condition. The story is a sad one, but thinking of myself as potentially in the same category as an NBA basketballer made me feel just a little more chirpy, especially since my sports-playing history is a tale of great aspiration and enthusiasm coupled with limited achievement.
The staff with whom I felt tension were financial representatives, who visited on several occasions, and called my cell phone (at one point while I was talking to a doctor) to try to get me to sign a payment form. If signed, the form committed me to paying all costs not covered by insurance. The staff pursuing my signature were friendly. And it wasn't surprising to me to be told about these forms during my stay. But I couldn’t help but be slightly sickened by this constant reminder of the links between money and access to emergency treatment in the US. I was determined not to sign the form, so I asked on several occasions for more time to consider my position, and eventually the representatives must have given up on me, or forgotten about it. A form remained unsigned on the side of my bed when I was discharged – a small, maybe meek, symbol of my opposition to the forces of finance driving healthcare.*
Before I was discharged I spent two nights in a smaller room that I shared with a middle-aged man, Joe, who was about to get heart surgery. I didn’t see much of Joe, a slightly taciturn but seemingly kind guy who was a doctor himself, since a curtain remained drawn between our beds. But I heard a lot about him: you cannot avoid learning about other people through overhearing conversations in hospital rooms like that one. One of the first things I heard was a panicked scene when I woke at 5.55am on a Wednesday morning to hear, five minutes before his surgery, Joe apparently losing consciousness. His wife shouted, “Joe! Joe!” and cried for help, with monitors beeping loudly in the background like they do in television and movies. Joe recovered, fortunately, but his surgery was delayed, and the incident was a sharp reminder of what heart surgery might entail.
It was around this time I also learned - through overhearing Joe’s family, and some Googling - that a patient was being tested at Mt Sinai for Ebola. That didn’t do anything to reduce my anxiety. I started wondering whether I could have come into contact with the man on my first day in the emergency ward, or indirectly through my visits to reception desks and shops down the corridor. I soon realised that this kind of speculation wasn’t all that rational, or helpful.
My own medical position appeared to be stable - apart from several moments of brief chest pain, which may have been the result of anxiety - and the doctors were closing in on a diagnosis. After a gentle older cardiologist, Dr. Halperin, spotted a strange double flap at the back of my throat, called a bifid uvula, the medical teams started to favour not Marfan Syndrome but a slightly more aggressive and newly-discovered syndrome called Loeys-Dietz Syndrome. Loeys-Dietz is another connective tissue disorder, which often manifests through long limbs and spidery fingers, but also involves certain specific symptoms – a bifid uvula, flat feet (which I have), and aortic enlargement. Doctors are keener to operate on those with Loeys-Dietz Syndrome, when the aorta is less enlarged than with Marfan Syndrome (for Marfan the threshold for surgery is a 5cm diameter in the US, I was told whereas the American threshold is 4.5cm for Loeys-Dietz), since the danger of a tear is greater. This made the accurate measurement of my aortic enlargement all the more important: my first measurement had come back at 4.9cm on the CT scan, whereas my second measurement on my echo had been 4.1cm.
To clarify the measurements, I had to do MRA imaging of both my brain and my heart. Getting an MRA done is a strange experience, as anyone who has had one will know. You lie on a slab, with your chest or head fixed in place, and you enter a large dome. Odd sounds are emitted, which reminded me of the robot voices on the Daft Punk song, Technologic. And the technician issues various instructions over a loudspeaker-like instrument, including “breathe!” and “breathe normally!”. To avoid becoming too anxious about it, I again played Liam Finn’s Second Chance in my head. The rippling synthesizer sounds and scratching guitar tune kept me calm, and I tried to write out the words in my mind: “Sew the seeds/Sew the seeds to life/By packing up to make it right.” I thought also of the people that had made the previous days bearable – my family and girlfriend, who were constantly in contact; my visiting friends; and the virtual visits I received on Skype from people in the UK and New Zealand (including a wonderful group Skype call with the friends with whom I’d organised a conference in Oxford, the Global Scholars Symposium).
Following a long wait, the MRA results came back: showing an enlargement of 4.5cm – right on the threshold of surgery. To my surprise, the doctors were confident about discharging me. I asked them to hold off on letting me go so quickly, partly because my girlfriend Julia and mum were now on their way to be beside me, and partly because I had earlier been told that if I had Loeys-Dietz, I may need surgery at this level of enlargement. After some further discussions, my discharge recommendation was confirmed – and I was encouraged by the very thorough Dr. Kontorovich to get genetic testing, since a Loeys-Dietz diagnosis could only be clarified with this genetic information.
Max after being discharged from hospital.
Leaving the hospital was in some ways a sad experience. I took off the electrodes that had been stuck to my chest (leaving me with paintball-like shapes imprinted all over my chest), exchanged my hospital gown for the t-shirt I’d worn when I first came in, and got myself out of the bed I’d been in for days. As I walked out, I said goodbye to Joe. “I feel like I’ve gotten to know you quite well,” I said, “even though we haven’t talked much.” He smiled. “Goodbye, Max.” And I wrote notes on scraps of paper to the doctors and nurses who had been so supportive. My hospital experience was over, for now.*
My Mum and girlfriend, Julia (as well as a family friend, Lora), soon arrived in New York. It was wonderful to be surrounded by people, after long periods of solitude in the hospital – and having them close, as I slept or walked or read, gave me a sense of security, especially as my mind wandered to whether I could suffer a sudden fatal dissection (something that is a possibility, albeit a small one, given my aortic size and possible underlying condition). It was uplifting to get unexpected messages of support, and beautiful gifts to make me feel better: more flowers from Louis, a care package from Ronan, a book on Ambedkar from Eesvan.
Being out of the hospital and back at work has also been tough, however. In the hospital, I felt relatively healthy, comparing myself to elderly and self-evidently ill individuals all around me. But outside in New York, I see myself alongside apparently healthy and active people. I’m ashamed to admit it, but if I’m honest, I find myself feeling an occasional flash of jealousy when I watch others and assume (perhaps wrongly in some cases) that they have no health issues to worry about. More importantly, I have started to process the information that I received in hospital. I have wondered about the minute differences between a 4.5 and 5.0 aortic enlargement. And I have thought about how a Loeys-Dietz diagnosis might alter my future career plans and life – since, if confirmed, it would require care and monitoring and may have implications for whether I can have children.*
I got back on the Megabus on that desolate Thursday more than two weeks after the initial fainting episode, which ended up in Baltimore. I was there to see Dr. Dietz (one half of the team that discovered Loeys-Dietz Syndrome) and a surgeon specialist, Dr. Cameron. In Baltimore, I was told by Dr. Dietz at Johns Hopkins Hospital that it was pretty likely that I had Loeys-Dietz Syndrome, and I finalised plans for genetic testing. Dr. Dietz, a kind and attentive man, emphasised that if properly managed and operated on, individuals with Loeys-Dietz still lead long, successful lives (into their sixties and seventies), and he clarified some information that had made me worried earlier. One statistic that had scared me was that those with Loeys-Dietz have an average life expectancy of 26.1 years – my exact age in August 2014, the time of writing – but Dr. Dietz said that was a figure drawn from early cases of Loeys-Dietz; he had now seen a far broader spectrum of cases, which would change the statistic significantly. I had medication confirmed, and talked about surgery with the world expert, Dr. Cameron, who discussed options in the US, the UK, and New Zealand.
I’m waiting on the results of my genetic testing, finishing my internship, and preparing myself for surgery or managing my medical condition. One challenge to grapple with is the constant anxiety I feel that a dissection could be imminent. Is that numbness in my foot a product of bad circulation, traceable back to my heart? What about that neck pain – didn’t Charles De Gaulle have neck pain (as I have read) just before he died, possibly of a connective tissue disorder? And is that chest ache something problematic, or just my anxiety? These questions – rational and irrational – regularly intrude into my thinking, and I am trying to learn to let them pass. But at this point I cannot deny that they are at once distracting, unsettling, and sometimes terrifying.
I feel, alongside that anxiety, a great sense of gratitude and good fortune. What would I have done without the emergency health insurance provided by my place of study? Would I know all this if I hadn’t fainted that Sunday morning (something that the doctors still can’t explain, and which Dr. Cameron called “my guardian angel”)? Would I have even gone into hospital had Andrew not mentioned Marfan Syndrome in that apartment in Karachi eight months ago?
I’m trying right now, with gratitude and still some anxiety, to start to think about the future again. My sense of time compressed in hospital – I could think only of the coming hours. And I am still focused only on the day ahead. I have learned, I think, the true meaning of that hackneyed phrase, “one day at a time”. But as my confidence builds, I hope that I will be able to think more imaginatively about the arc of a life in front of me – a thought that has always given me excitement and happiness.*
So hearing about Marfan in Pakistan; blacking-out and Skyping the UK; if I was a donut/you’d wanna glaze me; Gladys Brodsky and the NBA’s Isaiah Austin; doing CTs and MRAs; hearing about Ebola in the background and Loeys-Dietz in the foreground; through Baltimore and Megabuses – that’s how I’ve got here, to where I am now.
“So it seems”, as that Liam Finn song goes. “So it seems tonight.”
Max Harris had successful heart surgery at Oxford in November 2014. Doctors say his long-term prospects are good.